UNL scientists are using MRI to monitor biomaterials and engineered tissues. Among other advances, some day this could lead to noninvasive biopsies of potentially cancerous tissues or regenerated organs.
Angie Pannier and Shadi Othman, UNL biological systems engineers, are studying engineered bone and fat tissues that in the future could be implanted into the human body to replace tissue lost due to injury or disease.
While tissue engineering isn't new - engineered skin and cartilage already are available in the United States - using an MRI to monitor growth and development is.
Othman is combining MRI with mechanical actuators and custom software to develop a technique called magnetic resonance elastography to measure changes in the mechanical properties of engineered tissues in living mice.
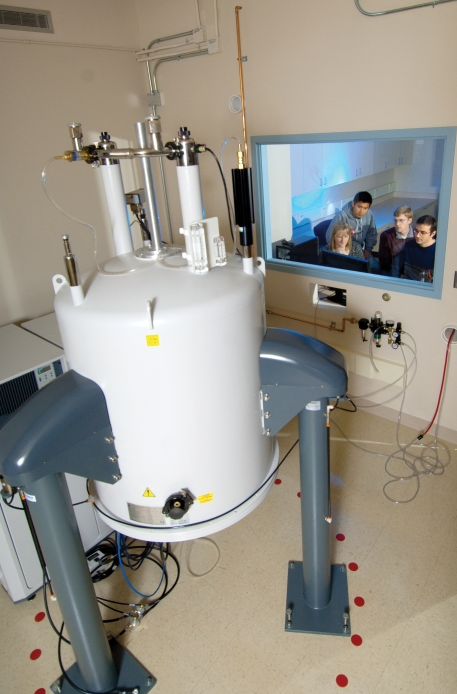
The biological systems engineering department received the 9.4 Tesla, high-field MRI scanner in December. Its use will be dedicated to basic biomedical engineering research and regenerative medicine.
"We are the first group in the world utilizing high field MRI to measure mechanical properties of living systems with very high spatial resolution," the Agricultural Research Division scientist said.
Othman is combining this technique with Pannier's tissue engineering research to image engineered tissues and biomaterial scaffolds used for tissue engineering. Biomaterials serve as a scaffold, or physical structure, on which to grow tissue. The cells grow on the scaffold to form a new tissue. Using magnetic resonance elastography, or MRE, Pannier and Othman can determine the stiffness of the engineered tissue without any damage to the tissue or mouse, a feat not possible with current technologies. In addition, they can study various other properties of the cells and biomaterial scaffolds, including water and molecular content.
MRE uses a mechanical actuator that creates a sonic excitation that travels in soft tissues, which then is monitored by MRI techniques.
For example, if tissue is stiff, the sonic wave will be longer, indicating a stiffer engineered tissue like bone, or in the case of cancer, a sign of a tumor.
Right now if a patient suspects cancer, the first thing a doctor does is determine how hard the tissue is. Based on feeling, the doctor would order a biopsy.
"With our technique, we can image the tissue and assess how stiff the tissue is in vivo. It would be a noninvasive biopsy," Othman said.
A cancerous tissue might give a different image than a normal tissue, said Jeyam Subbiah, biological systems engineer, while an engineered bone tissue would give a different image than an engineered fat tissue.
"Tissue engineering hasn't realized its potential because there are so many things we don't know or understand yet," Pannier said.
Researchers hope the MRI and more specifically MRE will answer some of these questions.
Othman takes the engineered tissue and implants it into mice, which then are placed in the MRI to monitor over time as the tissues grow.
Because the MRI allows scientists to monitor tissues while the mice are still alive, they can observe the tissues as they grow over time.
Othman is able to determine if growing tissues are getting stiffer like bone or softer like fat.
While researchers right now are only monitoring the tissue, in the future they will create a defect in a mouse, which will be replaced by engineered tissues, which can be monitored over time for changes in tissue growth and stiffness using MRE.
"We hope what we are doing here today will eventually be able to be done in a hospital some day," Othman said.
The Agricultural Research Division is a unit of the university's Institute of Agriculture and Natural Resources.
- Sandi Alswager Karstens, IANR News Service